Hearing Loss in children
Authors: David Horn, Hitomi Sakano
Hearing loss in children deserves special attention because of its significant impact on speech, development, and learning. Thus, an emphasis should be placed on early diagnosis and rehabilitation.
Depending on the occurrence age, deafness may be prelingual (before development of speech) or post-lingual (after development of speech). Peri-lingual deafness is when some speech has been acquired.
Prévalence
United States epidemiology: 0.14% infants screened are diagnosed with hearing loss, and 0.5% of children (age 3-17) are surveyed to have some degree of hearing loss .
Type
Hearing loss is typically categorized as follows:
2) Sensorineuronal (SNHL) Sound signals are not converted into neurological signals, often due to abnormalities of the inner ear (cochlea or auditory nerve).
3) Mixed Combination of the above.
For details on specific pathologies, see links under “Pathology” on the menu and “hearing loss” under General public.
Causes
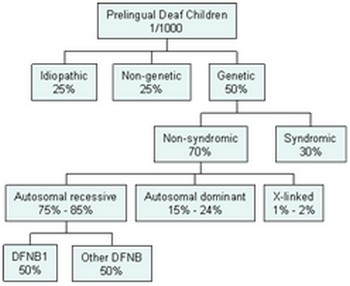
Diagram summarizing the causes of hearing losses in children.
Genetic ~50%
Genetic causes are classified to two categories:
1) Syndromic: associated with other congenital abnormalities. They account for ~1/3 of cases and include: Usher, Pendred, Waardenburg, Alport, Jervell, Lange-Nielson syndromes.
2) Nonsyndromic: represent the remaining ~2/3. The majority (70-80%) of these are inherited as autosomal recessive. ~1/2 are due to autosomal recessive connexin 26 and 30 mutations. Autosomal dominant mutations may present with post lingual progressive hearing loss with variable onset.
Note: There are over genetic 100 loci that are associated with inherited hearing loss. Lists and further information about each gene are available at http://hereditaryhearingloss.org
Nongenetic ~25%
The most common infectious cause of congenital sensorineuronal hearing loss is congenital cytomegalovirus (CMV) infection, with an incidence of 0.1-3/100 live births . Although most babies are asymptomatic, a few will develop progressive bilateral SNHL. The estimated prevalence of moderate-profound SNHL due to CMV is 0.2-0.6/1000 live births. Diagnosis of infection can be made by testing umbilical cord, serum or urine.
Idiopatic ~25%
Environmental and other nongenetic causes. Can be toxin or noise-induced, see links under “Pathology” on the menu and “hearing loss” under General public.
Les surdités génétiques représentent 50% des surdités congénitales.
Elles peuvent être syndromiques, c’est-à-dire associées à d’autres anomalies congénitales liées à une anomalie génétique. Elles représentent 30% des surdités génétiques et comprennent des syndromes comme le syndrome de Pendred, de Waardenburg, Alport, Jervell, ou Lange-Nielson.
Elles peuvent être non-syndromiques et représentent les 70% restants. La majorité des surdités non-syndromiques ont un mode de transmission autosomique récessif, largement représenté par les mutations des connexines 26 ou 30. Les mutations autosomiques dominantes ont des phénotypes cliniques plus variés avec des surdités de survenue plus variables en âge.
Remarque : il existe plus de 100 loci associés aux surdités génétiques. Pour de plus amples renseignements, vous pouvez vous reportez au site suivant http://hereditaryhearingloss.org
Les surdités non-génétiques représentent 25% des étiologies de l’enfant.
Parmi elles, l’infection congénitale au cytomégalovirus (CMV) présente une incidence de 0,1 à 3 pour 100 naissances vivantes. La majorité des enfants atteints sont asymptomatiques mais cependant, un certain nombre développera une surdité neuro-sensorielle progressive pouvant être bilatérale et sévère. Des anomalies neurologiques peuvent être associées. Le diagnostic est fait sur prélèvements sanguins ou urinaires.
D’autres causes sont une prématurité, un séjour en réanimation néo-natale…
Les surdités idiopathiques représentent 25% des étiologies de l’enfant.
Elles pourraient être environnementales ou liées à des causes non-génétiques comme des toxines.
How to identify hearing loss in children
Post-natal screening for hearing loss depends on each country. Ideally it should be performed before the age of 1 month using brainstem auditory evoked responses (BAER) or otoacoustic emissions (OAE). Those infants diagnosed with hearing loss, if confirmed by age 3 months-old, should be referred for appropriate medical/surgical/audiometric intervention prior to 6 months of age. There is evidence that earlier age of restoration of hearing results in better speech performance (see “critical period” in the cochlear implantation section below).
Clinical Workup/Diagnosis
Initial workup includes a full physical examination and audiometry (See “Audiometry” section on menu for details on diagnosis.) Further workup may include imaging (CT or MRI to determine anatomical abnormalities) and blood tests (if genetic or infectious causes are suspected). CMV testing of umbilical cord or newborn blood spot may be pursued if CMV is suspected as early treatment may stabilize the hearing loss.
Treatments
Treatment is tailored to the specific pathology of hearing loss and includes pharmacological, surgical or hearing amplification treatments. See “rehabilitation” and “Pathology” section of the menu for details on hearing amplification and cochlear implant technology. In the following sections, we will focus on cochlear implantation, particularly as it pertains to children with profound SNHL.