Cochlear implants: overview
Authors: Diane Lazard
Contributors: Sam Irving
Cochlear implants are devices that transform auditory acoustic information into electrical signals delivered directly to the auditory nerve. They are used mainly in cases of severe to profound bilateral hearing loss, notably in adults that have become deaf, and in children with congenital deafness, and offer the possibility of oral communication.
Now for some history!
The idea of reproducing auditory sensation using electrical stimulation was first suggested in the 18th century: The physicist Alessandro Volta passed a current of 50 V through metal rods that he had inserted into his own ear canals and described the perception of ‘a kind of crackling’ noise.
The first implant to stimulate the auditory nerve directly via a single electrode was used in France in 1957 (A. Djourno et C. Eyriès).
The results allowed the perception of sound, but not the understanding of speech. Further French attempts were carried out via an electrode inserted into the cochlea. Four years later, W. House, in California, carried out a series of surgeries where a single-electrode implant, similar to the French device, was inserted into the patients’ cochleae.
In 1964, B. Simmons began to develop a multi-electrode device containing six electrodes. Although unable to provide speech comprehension, his research demonstrated that using multiple stimulation sites permitted the pitch discrimination. The first single-electrode device was placed on the market in 1972 by W. House.
In 1976, back in France,Pialoux, Chouard and MacLeod, publish the results of a study using an 8-channel implant which offered to patients the comprehension of 50% of test words without the use of lip reading. This work concludes with the commercialisation of the first multi-channel cochlear implant, in France. At the same time, other teams are also busy developing multi-channel implants in Austria (I. and E. Hochmair, “Med-El®“) and in Australia (G. Clark, “Cochlear® Ltd”)
In 1988, a consensus is reached under the National Institute of Health (NIH, USA), which favours the use of multi-channel devices at the expense of those with a single channel. At this time, it was estimated that 3000 patients were already benefiting from the use of a cochlear implant. In 1995, 12000 people had been implanted, in 2008, 120000 and in 2012 this figure had reached 200000 and continues to rise to this day.
Cochlear implants: how do they work?
External component:
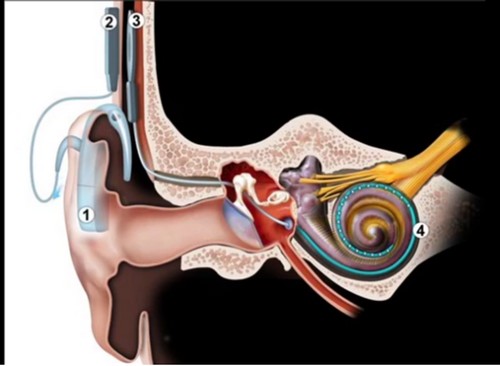
A speech processor (1) captures sounds via a microphone and converts them into an electrical signal, which is then transmitted across the skin by a transmitter (2) to the internal component (3)
Internal component:
The implanted part of the cochlear implant is a receiver-stimulator (3) that receives the signal from the speech processor and sends the electrical signal to the electrode array (4) situated within the cochlea. The latter’s role is to emit electric pulses that stimulate the fibres of the auditory nerve. The nervous signal that this creates is sent to the brain where it is analysed and interpreted.
Implantation procedure
The implantation of a cochlear implant has been standardised: under general anaesthetic, the round window is exposed by “posterior tympanotomy”, i.e. opening the bone between the facial nerve and chorda tympani nerve by mastoidectomy (removal of the air cells located behind the middle ear). The cochlea is then opened by cocheleostomy (drilling a small hole into the boney wall) or incision of the round window membrane and the electrode array is inserted.
The ideal placement of the electrode carrier is inside scala tympani. Insertion into scala vestibuli or insertion from scala tympani to scala vestibuli has been shown to decrease cochlear implant performance.
Activation of the cochlear implant does not happen immediately, as the skin needs to heal first. The activation delay depends on the surgical team and can vary from 10 days to a month or more.
Implantation criteria and aftercare
The decision to implant, the surgery and patient aftercare are carried out by a multidisciplinary team, generally composed of ENT surgeons, speech and language therapists, audiologists and psychologists. The degree of hearing loss, age, and the desire to communicate orally, as well as other potential issues (such as autism or ADHD) are all taken into account before the decision is made to implant.
The current criteria for implantation in the UK are ( www.bcig.org.uk):
- severe to profound hearing loss in both ears (defined as hearing only sounds that are louder than 90 dB at frequencies of 2 and 4 kHz without the use of hearing aids)
- little or no benefit from using a regular hearing aid
- have a desire to be part of the hearing world
- have no medical counterindications
In the case of a congenitally deaf child, early implantation is recommended to allow the auditory neural pathway to develop in a normal time-frame. If the education has been oralist (i.e. using oral communication and lip reading), there is no counter-indication for implanting a child or young adult with a congenital hearing loss. In older children, cochlear implant use may be less effective than in children implanted at an early age.
In adults, all individuals that present with post-lingual deafness that fits into the audimetric criteria can be fitted with a cochlear implant. There are no age limits if all other implantation criteria are met.
Bilateral implantation is carried out in certain cases. In the UK, simultaneous implantation is recommended for children and people who are also blind. Sequential implantation is not recommended in the UK, although these criteria vary depending upon the country where the implantation is to occur.
It is recommended that, in the case of unilateral cochlear implantation, the contralateral hearing aid still be worn so long as there are still benefits for doing so (even minimal). The implant and the hearing aid provide complemetary auditory cues, and benefit can therefore be observed with the use of both devices.
Risks:
- Meningitis (< 0.2%), avoided by a systematic vaccination before surgery
- Facial paralysis (< 0.7%), avoided by nerve monitoring during surgery
- Skin necrosis and exposure of the internal component
- local infection
- device failure
Rehabilitation
Speech understanding with a cochlear implant requires time and rehabilitation to integrate the received auditory signals. This rehabilitation is carried out with a speech and language therapist, an audiologist, but also on a daily basis by personal exercises (CD, internet, listening to sound environments…).
Results and limits of the cochlear implant
Aside from the implantation criteria, the implant has perceptual limits. Generally, speech comprehension in silence is attain by the vast majority of implant patients (90% success rate): some implantees can use the telephone and speak numerous languages!
However, a conversation in a noisy environment and music perception are difficult auditory situations. For example, listening to music gives rise to distinct feelings: come patients are able to appreciate it, and recognise some lyrics and melodies, whereas others will have great difficulty in doing so.
Limited success can be attributed to numerous factors. The usual clinical factors (age, duration of hearing loss, use of hearing aid, etc…) can only explain 22% of the variance of the results. Brain plasticity therefore plays a substantial part: beneficial when deaf subjects are turned to orality, negative when they use compensation mechanisms based on their sight (primary use of written and sign languages).